We specialise in identifying and helping to treat Dry Eye Syndrome
What is Dry Eye?
Dry eyes can be itchy, sore, gritty, red and even excessively watery. Dry Eye sensations are caused by problems with the tear film that form on the front of your eye and protect it from debris
The typical symptoms you may experience with dry or watery eyes include:
- Burning, stinging or itching, gritty feeling, irritation from wind or smoke, blurred or smeary vision, tired eyes, red eyes, excessive watering, light sensitivity and also contact lens discomfort.
The symptoms are often worse first thing in the morning or later in the evening and can be exacerbated by driving, computer use or air conditioning.
Common causes of Dry Eye?
There are a wide variety of reasons why you may suffer with dry eyes including:
- Ageing
- Hormonal changes especially in women
- Blepharitis
- Dry environment
- Prolonged computer use
- Systemic conditions such as arthritis
- Certain medications
- Contact lenses
- LASIK surgery
- Diet
There are lots of reasons why your eyes can become dry, and the aim of the dry eye clinic is to establish the main cause for your discomfort. Previous eye injuries or other problems within the body such as arthritis can increase dry eye disease. Disorders of the eyelid can also impair the complex blinking motion required to spread tears.
Your Dry Eye Consultation.......
Appointment Length 90 Minutes
Dry eye disease has become one of the most common eye conditions, with recent studies suggesting that 40% of people over 40 suffer with the condition. Our in depth 90 minute consultation involves diagnosing the type(s) of dry eye you may have, what the cause could be and discussing treatment options.
Airedale Opticians are one of a handful of Optometrists in the north of England, to have invested in state of the art equipment to help not only diagnose, but also invested in treatments to provide long-term relief for dry eye sufferers.
DIAGNOSIS – There is no single test that can accurately diagnose dry eye. We spend a large proportion of the time discussing your symptoms, triggers, history, health, occupation, diet and range of other detailed questioning to understand you and your dry eyes.
We have invested in one of the latest diagnostic equipments by Topcon called a Myah.
The Topcon Myah typically includes several tools for dry eye assessment, including:
- Questionnaire – We will use the OSDI questionnaire to ‘grade’ your dry eye which also helps with follow-up appointments.
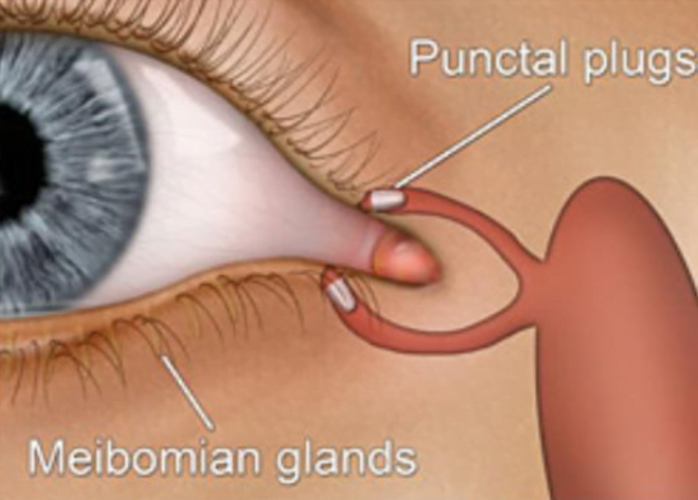
- Meibography: Captures images of the meibomian glands to assess their structure and function, which is crucial in diagnosing meibomian gland dysfunction (MGD), a common cause of dry eye.
- Pupillometry: Measures pupil size and dynamics, which can be informative in evaluating tear film stability and ocular surface health.
- Tear Film break-up time: Assessing tear film quality and stability.
- Tear Meniscus height: Assessing tear volume retained in the eye.
- Blink Analysis: Analyzes blink patterns and frequency, which can provide insights into ocular surface health and tear film dynamics.
- Corneal Topography: While not directly related to dry eye assessment, corneal topography can still be valuable in identifying irregularities on the corneal surface that may contribute to dry eye symptoms.
- Inflammadry:
InflammaDry® is the first and only, rapid, in-office test that detects MMP-9, an inflammatory marker that is consistently elevated in the tears of patients with dry eye disease. Other dry eye tests only measure tear production and stability. InflammaDry accurately identifies patients with dry eye allowing for optimal treatment methods and better quality of life.

Dry Eye Treatments Available at Airedale Opticians
We offer a variety of Dry Eye treatments in-house. We now offer the revolutionary IPL/LLLT treatment (see details below).
We can provide tear duct syringing which can break down and remove blockages in the tear ducts. We can also fit Puctum Plugs, tiny plugs that fit into the tear ducts and avoid excessive drainage of the tears.
All of these procedures can be carried out by one of your trusted optometrists, in practice, at a date and time that suit you, no doctor or hospital referrals are required. See our Fees Page for pricing details.
Intense Pulsed Light (IPL) and Low Level Light Therapy (LLLT)
Current treatments for Dry Eye treat the symptoms to enable you to be more comfortable. However, there is a now a treatment available which treats MGD (Meibomian Gland Dysfunction), the cause of up to 80% of dry eye cases.
IPL (Intense Pulse Light) treatment combined with LLLT (low level light therapy) is a pain-free and effective way to treat dry eye conditions related to MGD, improving tear quality and other symptoms reported by patients
How Does IPL/LLLT Work?
IPL causes photocoagulation (it closes these abnormal vessels) and also photorejuvenation of the skin cells. IPL treatment also opens up the meibomian glands and liquifies of the oil within the glands.
How quickly does it work?
Costs of Treatment
-
Dry Eye Assessment £249
Dry Eye Investigation with Topcon Myah, Diagnosis & Treatment Plan. Includes Inflammadry & one follow up appointment.
-
IPL (Intense Pulsed Light) & Meibomian Gland Expression £795
4 Sessions of IPL including Meibomian Gland Expression after each IPL Treatment
-
IPL and LLLT One- Off Treatment £200
Following initial treatment of IPL and LLLT - This is the cost of one-off IPL & LLLT (Includes Gland Expression)
-
IPL Stye/ Chalazion Treatment £200
One treatment with IPL and LLLT. 2 Courses maybe required
-
LLLT Low Level Light Therapy Top Up Treatment £100
Ongoing LLLT after Initial Treatment
-
Zest Treatment for Ocular Inflammation £160
Intense Zest Treatment to help bring Eye inflammation under control quickly
-
Blephex Blepharitis Treatment £95
Eyelid debridement (cleaning) treatment to intensely clean the eyelashes from Blepharitis
-
Dry Eye Assessment Follow Up £85
Follow up appointments within 6 months of original appointment
Other Treatment Options
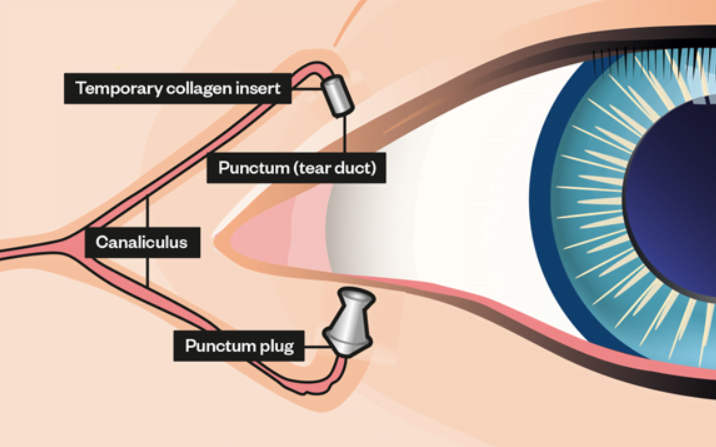
Punctum Plugs
Punctal plugs are small devices that are used to block the tear drainage channel in the inner corner of your eye. The plugs are inserted into the tear duct opening, which is called the puncta. Tears normally drain out from this channel through the back of your nose and into the back of your throat. The punctal plug acts as a dam by preventing tears from flowing out. This helps keeps your eyes moist with your own tears. They can also help artificial tears last longer.
Punctal plugs can be inserted for a short amount of time or permanently. Temporary punctal plugs are typically made out of collagen, a material that is found in bone and skin. These plugs naturally dissolve over time. Permanent punctal plugs are usually made out of silicone.
How Are Punctal Plugs Inserted?
Punctal plugs can be inserted in the lower eyelid, upper eyelid, or both. Before your eye care practioner inserts a plug, he/she will measure the opening of your tear duct to determine the size of plug that you will need to block your tear duct. He/she will sometimes use topical anesthetic drops (numbing drops) before the procedure, but in many cases, no anesthesia is needed. The exact way your eye care practioner inserts the plug depends on the design and shape. Some plugs come with special inserters, but other types are inserted with forceps or other instruments. The location of insertion also depends on the type of plug. You can see some plugs after they are inserted. Others are inserted deeper into the tear duct and will not be visible when you look in the mirror.
You may have some mild discomfort while the punctal plugs are inserted, but it will be very brief. Most people cannot feel the plugs once they are in place. If they do feel them, it is a mild sensation that is not bothersome. You can resume normal activities and drive yourself home immediately after the procedure.
How Are Punctal Plugs Removed?
Temporary punctal plugs dissolve naturally and do not require removal. Permanent punctal plugs do not need to be removed unless you are bothered by them or develop an infection (which is extremely rare).
Removing punctal plugs is usually very easy. Your eye care practitioner may take out the plug using forceps. If the punctal plug has migrated deeper into the tear duct and cannot be removed with forceps, the plug can be flushed out using saline solution.
What are the Risks of Punctal Plugs?
Punctal plugs rarely cause serious side effects, but they do have some risks. Possible risks include:
- The plug falling out, this is the most common problem
- Excessive tearing, the plugs can be removed if this happens
- Eye infection, the plug can be removed if this happens
Flow Controllers
Flow controllers are a tiny hollow insert which are placed in the tear duct, holding it open.
These Flow Controller plugs are used for draining tears in the treatment of Epiphora caused by zero flow while the rest of the lacrimal duct is normal and keeps a blocked punctum open assuring normal tear regulation.










